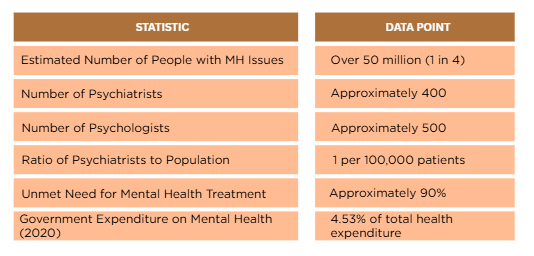
Pakistan is grappling with a silent but staggering mental health crisis. Over 50 million people—approximately one in four Pakistanis—experience some form of mental health challenge. This crisis is driven by a constellation of stressors such as political and economic instability, recurring natural disasters, persistent conflict and security concerns, deep-seated poverty, social inequality, and the psychological toll of rapid urbanization. Prolonged exposure to these conditions erodes individual resilience, leaving many vulnerable to psychological distress.
The situation is further exacerbated by a critical shortage of mental health professionals. With just 500 psychologists and 400 psychiatrists serving a population of over 240 million, access to care is alarmingly limited, particularly in child and adolescent psychiatry. Compounding this is a lack of standardized mental health training across the healthcare workforce, and severely underfunded services, where available resources are overwhelmingly directed toward reactive treatment rather than proactive, preventative care.
Global Guidance and Local Application
The World Health Organization (WHO) offers a robust, adaptable framework for addressing mental health in low- and middle-income countries (LMICs). Central to this approach is the concept of community-based care, which empowers non-specialist individuals with the tools to provide early-stage mental health support. This “task-shifting” model not only mitigates the shortage of mental health professionals but also enhances accessibility, particularly in rural and underserved areas.
In Pakistan, lay counselor programs have demonstrated promising outcomes. Trained community members provide frontline support, referring complex cases to specialists when needed. Digital counseling initiatives, led by community health workers, have expanded the reach of care to marginalized populations. These efforts underscore the potential of a localized, culturally sensitive mental health infrastructure rooted in community empowerment.
Progress is also visible at the institutional level. Government initiatives such as the Umang helpline, offering 24/7 mental health assistance, and school-based mental health projects have gained momentum. The President’s Initiative on School Mental Health focuses on training teachers to identify and respond to early warning signs. Additionally, Pakistan has piloted the WHO School Mental Health Programme, yielding encouraging outcomes in teacher mental health literacy and classroom support strategies.
Adolescence: A Critical Window for Intervention
Even within this challenging landscape, strategic points for intervention exist, and adolescence provides a critical window of opportunity. This stage of development is marked by profound physical, emotional, and social changes. It is also a period of heightened risk for the onset of mental health disorders, with many individuals experiencing mental health challenges for the first time. Therefore, interventions during adolescence hold the potential to significantly alter the trajectory of a young person’s life, promoting positive mental health and preventing the escalation of difficulties.
While there is a growing awareness of mental health issues among young people, this increased understanding is not always accompanied by access to adequate resources. Research has indicated that heightened awareness without readily available support systems can paradoxically worsen mental health. This suggests that simply informing young people about mental health is insufficient; it must be coupled with the provision of accessible and appropriate support mechanisms to avoid causing further distress or a sense of helplessness.
Conversely, the presence of healthy interactions and
strong bonds within the family can serve as critical protective factors against mental health challenges.
A nurturing environment characterized by acceptance, warmth, and support plays a vital role in building resilience and promoting healthy mental development during this crucial stage.
Preventative Care in Action:
A Model from Cedar College
Rather than seeking entirely novel interventions, Pakistan can benefit from adapting proven models to fit its local context. One such example is Cedar College, which has developed a mental health curriculum drawing from Dialectical Behavioral Therapy (DBT), Cognitive Behavioral Therapy (CBT), and Dynamic Emotion Integration—all tailored to the lived realities of Pakistani students.
This program is built on the understanding that life inevitably presents stressors to everyone, and the ability to develop coping skills should not be limited to those in therapy. Equipping individuals early with the capacity to regulate their thoughts and physical responses cultivates robust resilience, allowing them to navigate ongoing difficulties with strength and unwavering resolve, rather than faltering.
Structured over 24 weeks, this program begins with the fundamentals of mindfulness, where students learn the essential tools to regulate their minds and bodies, laying the foundation for self-awareness and self-regulation. From there, the program focused on promoting personal growth by cultivating inner strength and building self-esteem. Lastly, students delved into understanding emotions, shifting away from labeling them as “good” or “bad” and instead learning to listen to the wisdom within each one. Emotions act as messengers, offering insights into our inner and outer worlds, and our role is to understand their meaning and respond with intentional, informed action.
Toward a Culture of Preventative
Mental Health
Pakistan’s mental health crisis is vast—but not insurmountable. There is no shortage of evidence-based models; what is needed now is collaborative momentum.
The true challenge lies not in a scarcity of effective models, but in fostering a collaborative ecosystem within Pakistan where institutions transcend siloed operations and competitive mindsets. Instead, a paradigm shift towards the open sharing of resources, evidence-based strategies, and collective expertise is crucial to expand the accessibility of mental health care preventative measures. Embracing the spirit of partnership and mutual support can cultivate a more resilient and mentally healthy community.
perinxavari@gmail.com